Raynaud’s symptoms ceased in a woman after treatment with hydroxycarbamide returned her platelet count to normal, according to a case study published in the journal of Case Reports in Medicine.
The study, “Myeloproliferative Disease: An Unusual Cause of Raynaud’s Phenomenon and Digital Ischaemia,” suggests Raynaud’s symptoms can appear as secondary to blood disorders.
In this case, a 59-year-old woman suspected of having vasculitis — a disease caused by blood vessel inflammation — suffered from several attacks of Raynaud’s phenomenon. These attacks were triggered by cold and affected her fingers and toes. The woman showed discoloration of her left and third toes with ischaemic lesions and pain, but doctors did not find any other symptoms of connective tissue disease.
Initially, she was given medication to improve peripheral blood flow and to control pain, but the treatment failed to improve her toes or stop the Raynaud’s symptoms.
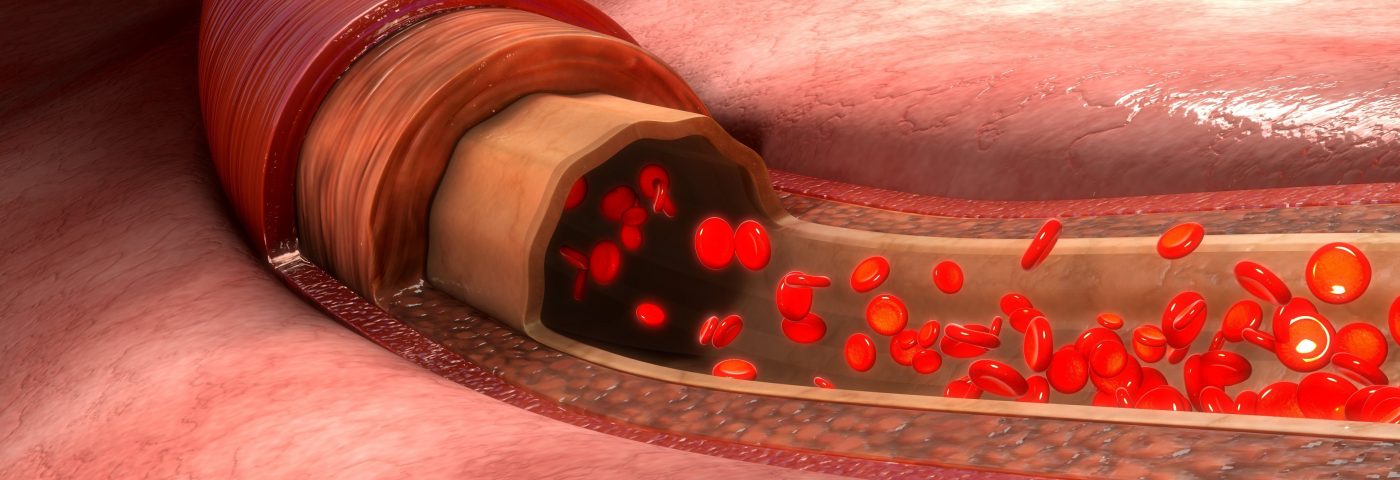
A blood analysis revealed an unusually high number of platelets (786 × 109/L; the condition is known as thrombocytosis) compared to the normal counts (150–400 × 109/L), and also a higher number of white blood cells. Doctors also found that the woman had a gene mutation identified in 50–60% of patients with essential thrombocytosis (ET), the JAK2 V617F mutation. ET is a chronic myeloproliferative disorder characterized by abnormal proliferation of blood cells.
Based on an ET diagnosis, the patient started treatment with hydroxycarbamide, a drug given to control platelets counts. After three months, her platelet values normalized and led to complete resolution of her Raynaud’s symptoms and healed the ischaemic lesions.
Another 268 patients with ET were then examined, but only one showed Raynaud’s phenomenon, indicating it is a rare manifestation in these patients.
Importantly, this study demonstrates that treatment of an underlying disorder can stop Raynaud’s symptoms.
Raynaud’s “is commonly a primary disorder but can be secondary to other conditions,” the team wrote. “Whilst the underlying cause in this case was unusual it emphasizes the importance of considering secondary causes which may not have an autoimmune aetiology.”
The authors suggest that the blocking of microcirculation by platelets might be a factor in ET that is associated with Raynaud’s. They highlighted that this case could alert doctors to investigate Raynaud’s phenomenon as secondary to other blood diseases. Monitoring blood cell counts in patients could identify myeloproferative disorders that can be treated together with Raynaud’s symptoms.