A recent review discussed the current and possible future applications of infrared thermal imaging (IRT) to diagnose Raynaud’s phenomenon. The authors believe this method can be introduced in clinical practice and provide low-cost diagnosis for patients with the condition.
The review is titled “Infrared Thermal Imaging In Connective Tissue Diseases” and was published in the journal Reumatologia.
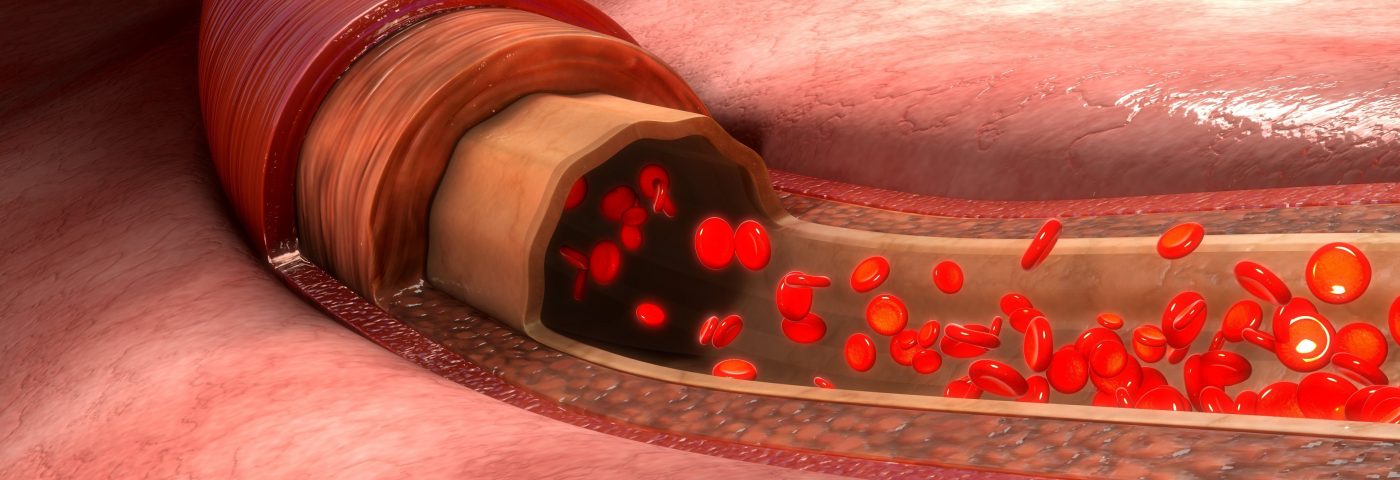
IRT is a noninvasive technique that allows the measurement of surface body temperature, and provides an overall assessment of blood circulation in small blood vessels.
This method has been used for several years to diagnose Raynaud’s phenomenon and systemic sclerosis (SSc), two conditions characterized by blood vessel abnormalities. In SSc, IRT has a potential role in assessing disease activity and monitoring treatment response.
The tool used most often for the diagnosis of different forms of Raynaud’s phenomenon is nailfold videocapillaroscopy (NVC), which allows the observation of the blood vessel’s structure. However, this method is not reliable to distinguish between a patient with Raynaud’s phenomenon and a healthy subject, as the obtained blood vessel images look similar.
Several studies have supported the use of IRT in detecting Raynaud’s phenomenon.
“In healthy subjects, the fingers, especially the fingertips, are usually warmer than the hand,” researchers wrote. “In [Raynaud’s phenomenon] patients the fingers are significantly colder than the hands, even between … episodes [of reduced local blood flow].”
This difference in temperature can be detected by IRT, and thus help clinicians make a proper diagnosis of their patients.
However, IRT may provide ambiguous results, mainly due to the absence of a standard protocol procedure and the low availability of appropriate equipment in the clinic.
“While the role of IRT as a single study in [Raynaud’s phenomenon] diagnostics remains ambiguous, it is a powerful complement to NVC,” researchers wrote. “Combining information about blood vessel structure from NVC with functional evaluation of microcirculation was proven to have better specificity and sensitivity in [Raynaud’s phenomenon] differential diagnosis than NVC alone.”
Also, several factors may influence the results of an IRT test, so both the test room and the patient need to be prepared.
“The ambient room temperature should be stable between 18°C and 25°C, optimally 22–24°C,” researchers wrote. “If it is too cold, [this] will cause vasoconstriction [narrowing of the blood vessels], and too much heat may cause excessive sweating, both of which alter the study outcome.”
Before the test, the patient should be acclimatized to the room’s temperature for at least 15 minutes. In the four to six hours before the test, patients should not smoke, drink alcohol, coffee, or tea, eat large meals, use cosmetics or other products in the region to be analyzed, or perform physical activity (including physiotherapy and massages), as all these factors may also alter the behavior of the blood vessels.
“Despite certain limitations, thermal imaging can find a place in clinical practice, and with the introduction of small, low-cost infrared cameras, possibly become a part of routine rheumatological evaluation,” the researchers concluded.